Tell us about your first few months working on coronavirus and the ground-breaking discoveries at the University of Bristol
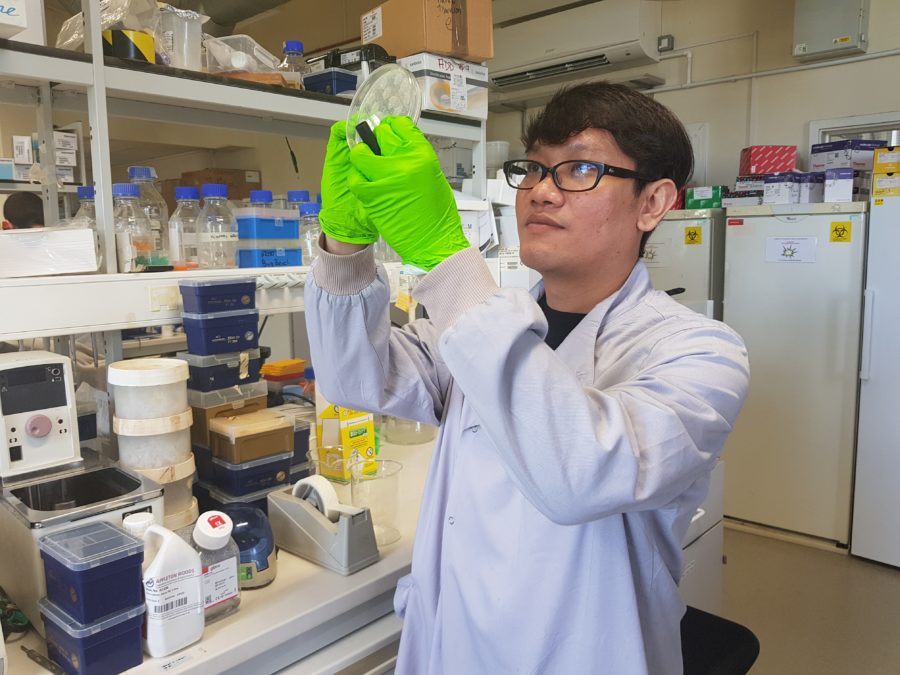
Andrew Davidson
Just after Christmas I had dinner with a Chinese research colleague. We discussed the virus outbreak in Wuhan. I was interested as I’ve worked on coronaviruses since 1999, including the 2002 to 2004 SARS epidemic. The next day he was recalled to his lab in China. He confirmed it was a type of coronavirus named SARS-CoV-2, the virus that causes COVID-19.
Over the past 4 years at the University of Bristol we have been establishing containment facilities to work on potential virus outbreaks. These facilities, and our experience with live coronaviruses, meant we’re quickly granted permission to work on the live COVID-19 virus. At that point we were the only academic research group with permission to work with the live virus in the UK.
In just under five weeks we got the virus and submitted our first paper. Usually it takes many months to deliver these results. This is one of the proudest moments in my career. It was the first paper in the world to describe molecular biology work with the live coronavirus. Read the ground breaking paper here.
David Matthews
Our early work changed the way people thought about how to grow and work with COVID-19 in the laboratory. Teams all over the world contacted us to collaborate and said our data had encouraged them to start working on COVID-19. Our basic research has helped scientists globally. For example, we validated inactivation strategies that have allowed big testing centres to develop protocols and safely advance their work.
Why has coronavirus become a pandemic? What is different about it to other viruses?
Andrew Davidson
We’re constantly telling students to watch out for the next pandemic. We’re globalised and we’ve upset the environment which creates the perfect conditions for any emerging virus. We’ve been expecting a global pandemic for years. We’d predicted a new strand of flu could infect a third of the globe in a year if left unchecked.
David Matthews
Coronavirus is different to other emerging viruses because it hits the sweet spot. It mostly doesn’t kill or impede people. Some people are unaware they even have it. This means it’s easily spreadable. Everyone is susceptible to it because we don’t have immunity yet. For some people it is particularly dangerous and can cause more serious disease. In a world of 7.8 billion people this makes for a disastrous outbreak.
How important is international collaboration to coronavirus research?
David Matthews
International collaboration is key to all scientific research. Disease is an international problem; it doesn’t have borders. coronavirus research is the same. There must be an international response. It’s been uplifting to see how the global science community has come together to work as hard and as fast as they can on coronavirus.
Andrew Davidson
We’re collaborating with teams all over the world, from China, to the US, to Australia, to Singapore, and Switzerland. Even in our small team we have PhD students from Saudi Arabia to Thailand who have been instrumental in driving forward our work. As a scientist you build up international contacts through conferences, international students, and overseas research. These contacts are vital in sharing resources and advancing findings across the world. Newton funding has been particularly instrumental in accelerating international research collaboration.
How do you see this ending, what’s the solution to the coronavirus pandemic?
Andrew Davidson
We need immunity to the virus. In the short term, this means we need vaccines. In the longer term, we need drugs. We’re currently working with the University of Oxford on vaccine development. We’re also researching the human immune response to understand what antibodies are produced when you are infected with coronavirus and which of these protects you against being infected again, and how long that lasts for.
David Matthews
The development of vaccines and drugs is complicated by our discovery that coronavirus can mutate when it is grown in the laboratory. This interferes with vaccine and drug research. For example, in vaccine trials with animals, the animals are first exposed to a small part of SARS-CoV-2 when they are vaccinated. After a few weeks they will then be deliberately infected with SARS-CoV-2 that has been grown in the laboratory. If that part of the virus mutates when it is grown in the laboratory then using it to infect the vaccinated animals will invalidate the vaccine trial. Our findings were immediately discussed at the World Health Organisation, and since have been used to encourage scientists worldwide to check that their virus samples have not mutated when doing vaccine research.
This is the first blog in a series of 2. In the next blog we speak to Adam Finn who leads the University of Bristol’s COVID-19 Emergency Research Group (UNCOVER). We’ll be exploring if infectious diseases are the world’s greatest challenge. Stay tuned.
Find out more about the work of Bristol University COVID-19 Emergency Research Group or via Twitter, @BristolUncover